Talk to Sales
How to Integrate Epic with Medical Billing Software: Complete Guide + Best Solutions
Epic EHR holds 41.3% of the hospital market and 43.92% of ambulatory care, making Epic-to-billing integration critical for revenue cycle success. This guide covers integration methods (FHIR APIs, HL7 interfaces, custom connections), step-by-step implementation, common challenges, and the top 5 Epic-compatible billing platforms to streamline claims, reduce denials, and accelerate reimbursement.
Why Epic EHR Integration Matters for Medical Billing
Epic Systems dominates the healthcare IT landscape with over 37.7% of U.S. hospitals and more than half of all inpatient beds using its EHR platform. For practices and health systems using Epic, seamless integration between clinical documentation and billing systems is essential to:
Key Benefits of Epic-Billing Integration
- Reduce claim denials: Automated data transfer eliminates manual entry errors that cause 60-70% of initial denials
- Accelerate reimbursement: Real-time eligibility checks and automated claim submission reduce A/R days by 15-25%
- Improve coding accuracy: Direct access to clinical documentation ensures proper CPT/ICD-10 code selection
- Minimize administrative overhead: Staff spend 40-50% less time on manual data entry and claim rework
- Ensure compliance: Automated audit trails and documentation linkage reduce regulatory risk
The global revenue cycle management market is projected to reach $105.35 billion by 2030, with Epic integration capabilities becoming a key differentiator for RCM platforms.
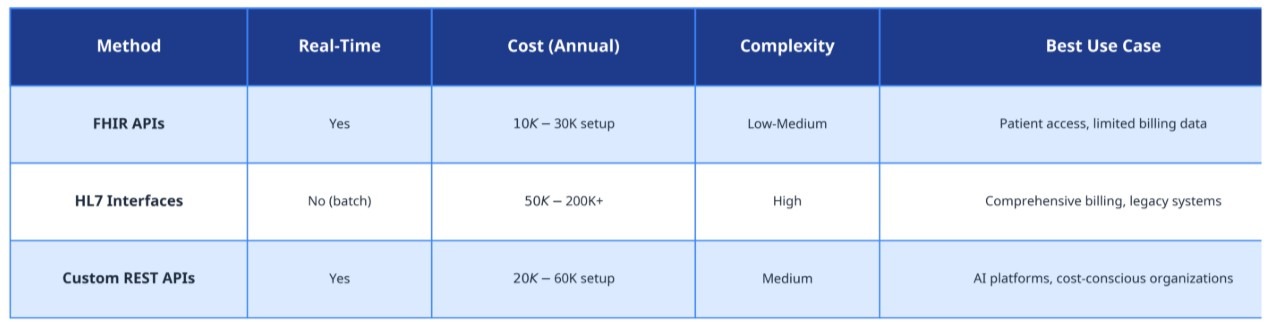
Understanding Epic Integration Methods
Epic offers three primary integration approaches for connecting to third-party billing systems. Each method has distinct advantages, complexity levels, and cost implications.
1. FHIR APIs (Fast Healthcare Interoperability Resources)
What it is: Modern, RESTful APIs that enable standardized data exchange between Epic and external applications.
Best for:
- Cloud-based billing platforms
- Real-time data synchronization needs
- Patient-facing applications requiring consent-based access
Pros:
- Industry-standard protocol (easier to maintain)
- Real-time data access
- Lower integration costs than HL7
- Patient-directed exchange capabilities
Cons:
- Limited to specific data types (not all billing data available via FHIR)
- Requires Epic version 2018 or newer
- May need supplemental integration methods for complete billing workflows
Typical Cost: $10,000-$30,000 for initial setup
2. HL7 Interfaces (Health Level 7)
What it is: Legacy messaging standard for batch data transfer between Epic and billing systems.
Best for:
- Comprehensive billing data transfer (charges, encounters, demographics)
- Organizations already using HL7 infrastructure
- High-volume claim processing environments
Pros:
- Supports complete billing data sets
- Proven reliability for 20+ years
- Works with older Epic versions
- Handles complex data structures
Cons:
- Expensive licensing fees ($50,000-$200,000+ annually)
- Batch processing creates delays (not real-time)
- Requires specialized HL7 expertise
- Difficult to troubleshoot and maintain
Typical Cost: $50,000-$200,000 annually + implementation fees
3. Custom REST APIs
What it is: Proprietary API connections developed specifically for Epic's data structures, bypassing HL7 fees.
Best for:
- AI-powered billing platforms requiring real-time access
- Organizations seeking to avoid HL7 licensing costs
- Practices needing flexible, customizable integrations
Pros:
- No HL7 licensing fees
- Real-time data synchronization
- Highly customizable to specific workflows
- Modern, maintainable architecture
Cons:
- Requires Epic IT team collaboration
- Initial development time (4-8 weeks)
- Vendor must have Epic integration expertise
- May require Epic App Orchard approval for certain use cases
Typical Cost: $20,000-$60,000 one-time development
Integration Methods Comparison Table
Step-by-Step Epic-to-Billing Integration Process
Step 1: Define Integration Requirements
Timeline: 1-2 weeks
Key Actions:
- Identify required data elements (demographics, encounters, charges, diagnoses, procedures)
- Determine update frequency (real-time vs. batch)
- Map Epic modules to billing workflows (Cadence scheduling, Resolute billing, etc.)
- Document current pain points (manual entry, claim errors, delay sources)
Stakeholders to Involve:
- Epic IT team or Epic-certified analysts
- Billing department leadership
- RCM vendor technical team
- Compliance and security officers
Step 2: Select Integration Method
Timeline: 1 week
Decision Criteria:
- Budget: HL7 requires ongoing licensing; FHIR/REST have lower recurring costs
- Epic Version: Older versions may require HL7; 2018+ supports FHIR
- Data Needs: Complete billing data favors HL7 or custom REST; limited data works with FHIR
- Timeline: FHIR is fastest (2-4 weeks); HL7 takes 8-12 weeks; custom REST takes 4-8 weeks
Common Challenges:
- Legacy system compatibility issues with outdated Epic versions
- Security requirements for patient data access
- Epic IT resource availability (often backlogged 3-6 months)
Step 3: Configure Epic Data Extraction
Timeline: 2-4 weeks
Epic Configuration Tasks:
- Set up Chronicles database queries for billing data
- Configure Clarity reporting database access (if using batch extracts)
- Enable FHIR endpoints or HL7 message types
- Establish secure data transmission protocols (VPN, SFTP, or HTTPS)
- Create test environment for integration validation
Required Epic Expertise:
- Epic-certified technical analyst (Resolute, Cadence, or Beaker depending on specialty)
- Epic Bridges or Integration Engine specialist
- Security and compliance team for BAA and HIPAA review
Step 4: Build Billing System Integration
Timeline: 3-6 weeks
Billing Platform Tasks:
- Develop data mapping between Epic fields and billing system fields
- Build transformation logic for code sets (CPT, ICD-10, HCPCS)
- Configure real-time eligibility verification
- Set up automated claim scrubbing rules
- Implement error handling and retry logic
Testing Requirements:
- Unit testing of individual data mappings
- Integration testing with Epic test environment
- End-to-end workflow testing (patient registration → claim submission)
- Performance testing for high-volume scenarios
Step 5: Pilot and Validate
Timeline: 2-4 weeks
Pilot Approach:
- Start with single department or specialty
- Process 50-100 test claims
- Compare against manual billing for accuracy
- Measure key metrics (claim acceptance rate, denial rate, time to submission)
Validation Checklist:
✅ Patient demographics transfer accurately (name, DOB, insurance)
✅ Encounter data includes all billable services
✅ Diagnosis codes match clinical documentation
✅ Procedure codes align with charges
✅ Modifiers apply correctly based on service context
✅ Claims submit to correct payers
✅ Denial reasons are captured and routed appropriately
Step 6: Full Deployment and Monitoring
Timeline: 1-2 weeks
Deployment Steps:
- Roll out integration to all departments/specialties
- Train billing staff on new workflows and exception handling
- Establish monitoring dashboards for integration health
- Create escalation procedures for integration failures
- Schedule regular integration performance reviews
Ongoing Monitoring Metrics:
- Data synchronization success rate (target: 99.5%+)
- Claim submission time from encounter close (target: <24 hours)
- Initial claim acceptance rate (target: 95%+)
- Integration error rate (target: <0.5%)
Common Epic Integration Challenges and Solutions
Challenge 1: Epic IT Resource Constraints
Problem: Epic IT teams are often backlogged 3-6 months with competing priorities, delaying integration projects.
Solutions:
- Partner with vendors offering turnkey integration: Platforms like ENTER provide custom Epic integration without requiring extensive Epic IT involvement
- Leverage Epic App Orchard: Pre-approved integrations reduce Epic IT review time
- Use FHIR when possible: Requires less Epic IT configuration than HL7
- Schedule integration during Epic upgrade cycles: Piggyback on planned system changes
Challenge 2: Data Mapping Complexity
Problem: Epic's data structures don't always align with billing system requirements, causing data synchronization issues.
Solutions:
- Create comprehensive data dictionaries: Document every Epic field and its billing system equivalent
- Implement transformation layers: Use middleware to convert Epic data formats to billing formats
- Establish data governance: Define authoritative sources for each data element
- Build validation rules: Catch mapping errors before claims are submitted
Challenge 3: Security and Compliance
Problem: Improper integration can expose sensitive patient data to security vulnerabilities.
Solutions:
- Execute comprehensive BAAs: Ensure all vendors have Business Associate Agreements
- Implement role-based access: Limit data access to minimum necessary
- Encrypt data in transit and at rest: Use TLS 1.2+ for transmission, AES-256 for storage
- Conduct regular security audits: Review access logs and integration points quarterly
- Enable audit trails: Track all data access and modifications
Challenge 4: Real-Time vs. Batch Processing
Problem: Epic's batch-oriented architecture conflicts with modern billing platforms' real-time needs.
Solutions:
- Use FHIR for real-time data: Patient demographics, eligibility, and appointment data
- Supplement with batch extracts: Nightly feeds for complete encounter and charge data
- Implement event-driven triggers: Epic can trigger real-time notifications on specific events (encounter close, charge entry)
- Build caching layers: Store frequently accessed data locally to reduce Epic queries
Top 5 Epic-Compatible Medical Billing Platforms
1. ENTER: AI-First RCM with Custom Epic Integration
Integration Method: Custom REST APIs (no HL7 fees)
Key Features:
- Custom Epic integration for any Epic version
- Continuous integration support (free EHR switches)
- 40-day implementation timeline
- Real-time eligibility and claim scrubbing
- 99.6% contract value collection rate
Best For:
- Organizations seeking to eliminate HL7 licensing costs
- Practices want full automation with minimal Epic IT burden
- Health systems are frustrated with slow payment posting
Pricing: Custom based on volume
2. Availity: Epic-Certified Clearinghouse
Integration Method: HL7 + FHIR APIs
Key Features:
- Pre-built Epic integration via App Orchard
- Real-time eligibility verification
- Claims management and denial tracking
- Patient payment portal
- Payer enrollment services
Best For:
- Organizations already using Epic for clinical workflows
- Practices needing clearinghouse + RCM capabilities
- Health systems with Epic IT support
Pricing: Transaction-based (typically $0.50-$2.00 per claim)
3. Oracle Health (Cerner): Native Epic Alternative
Integration Method: N/A (unified EHR + RCM platform)
Key Features:
- Seamless clinical-financial data flow
- Enterprise revenue cycle management
- Contract management and compliance
- Patient accounting and billing
Best For:
- Organizations considering EHR switch from Epic
- Large health systems want a unified platform
- Enterprises with dedicated IT departments
Pricing: Custom enterprise pricing ($1M+ implementations)
Note: Oracle Health is a competitor to Epic, not an integration partner. Included for comparison.
4. Waystar: Revenue Cycle Technology Platform
Integration Method: HL7 interfaces + FHIR
Key Features:
- Epic-certified integration via App Orchard
- Predictive denial management
- Prior authorization automation
- Payment estimation and patient engagement
- Claims and remittance processing
Best For:
- Mid-sized to large practices (20+ providers)
- Organizations with high prior authorization volume
- Health systems needing patient financial engagement tools
Pricing: Per-transaction or per-provider monthly fees
5. R1 RCM: Enterprise Revenue Cycle Outsourcing
Integration Method: HL7 interfaces (full-service model)
Key Features:
- End-to-end RCM outsourcing
- Dedicated Epic integration team
- Revenue integrity and compliance
- Patient access and scheduling support
Best For:
- Large hospitals and health systems (100+ providers)
- Organizations wanting to fully outsource RCM
- Enterprises with complex Epic implementations
Pricing: $420-$1,300 per provider per month
Considerations: High cost and long implementation timelines (6-12 months)
Epic Integration Best Practices
1. Engage Epic IT Early
- Schedule initial meetings 3-6 months before planned go-live
- Understand Epic's integration approval process and timelines
- Identify Epic-certified resources on your team or your vendor's team
2. Prioritize Data Quality
- Audit Epic data before integration (clean up duplicate patients, invalid insurance)
- Establish data governance policies for ongoing maintenance
- Implement validation rules to catch errors at source
3. Plan for Epic Upgrades
- Epic releases major updates twice yearly (May and November)
- Test integrations after each Epic upgrade
- Build regression testing into upgrade workflows
4. Document Everything
- Maintain detailed integration specifications
- Create runbooks for common issues and troubleshooting
- Document all data mappings and transformation logic
5. Measure and Optimize
- Track integration performance metrics weekly
- Conduct quarterly reviews with Epic IT and billing teams
- Continuously refine mappings based on denial patterns
Frequently Asked Questions
How long does Epic-to-billing integration take?
Integration timelines vary by method:
- FHIR APIs: 2-4 weeks for basic data access
- HL7 Interfaces: 8-12 weeks for comprehensive billing data
- Custom REST APIs: 4-8 weeks for full automation
Total project timelines including planning, testing, and deployment typically range from 40 days (ENTER's approach) to 6 months (enterprise HL7 implementations).
What does Epic integration cost?
Costs depend on integration method:
- FHIR: $10,000-$30,000 one-time setup
- HL7: $50,000-$200,000+ annually in licensing fees
- Custom REST APIs: $20,000-$60,000 one-time development
Many modern RCM platforms (like ENTER) include custom Epic integration at no additional charge as part of their service.
Do I need Epic IT team involvement?
Yes, but the level of involvement varies:
- Minimal: FHIR-based integrations with pre-approved App Orchard apps
- Moderate: Custom REST APIs requiring Epic endpoint configuration
- Extensive: HL7 interfaces requiring Chronicles queries and Bridges configuration
Choose vendors with Epic integration expertise to minimize burden on your Epic IT team.
Can I integrate Epic with any billing software?
Technically yes, but practical success depends on:
- Billing software's integration capabilities (API support, HL7 compatibility)
- Epic version (2018+ required for FHIR; older versions need HL7)
- Budget for integration development and maintenance
- Epic IT team capacity and willingness to support
Modern cloud-based billing platforms generally offer easier integration than legacy on-premise systems.
What data can I extract from Epic for billing?
Common billing data elements include:
- Patient demographics: Name, DOB, address, contact info
- Insurance information: Payer, policy number, group number, eligibility
- Encounters: Visit dates, providers, departments, service locations
- Charges: CPT codes, quantities, modifiers, charge amounts
- Diagnoses: ICD-10 codes with POA indicators
- Clinical documentation: Notes, orders, results (for coding support)
Data availability depends on Epic modules implemented (Cadence, Resolute, Beaker, etc.) and integration method chosen.
Conclusion
Integrating Epic EHR with medical billing software is essential for healthcare organizations seeking to reduce denials, accelerate reimbursement, and minimize administrative overhead. With Epic commanding over 40% market share in both hospital and ambulatory settings, choosing the right integration approach and billing platform partner is critical to revenue cycle success.
Key Takeaways:
- FHIR APIs offer the fastest, lowest-cost integration for basic billing data
- HL7 interfaces provide comprehensive data but carry expensive licensing fees
- Custom REST APIs deliver real-time automation without HL7 costs
- Implementation timelines range from 40 days to 6 months depending on method and vendor
- Top Epic-compatible platforms include ENTER (AI-first automation), Availity (clearinghouse), and Waystar (denial management)
Ready to Streamline Your Epic-Billing Integration?
The right integration approach depends on your Epic version, budget, data requirements, and automation goals. Modern AI-powered platforms like ENTER can deliver custom Epic integration in 40 days with no HL7 licensing fees, while traditional enterprise solutions may require 6-12 months and significant ongoing costs.
Next Steps:
- Audit your current Epic-to-billing workflow and identify pain points
- Determine which integration method aligns with your budget and timeline
- Request demos from 2-3 Epic-compatible billing platforms
- Engage your Epic IT team early to understand resource availability
- Pilot with a single department before full deployment


