Talk to Sales
Top 5 R1 RCM Alternatives for Healthcare Providers in 2025

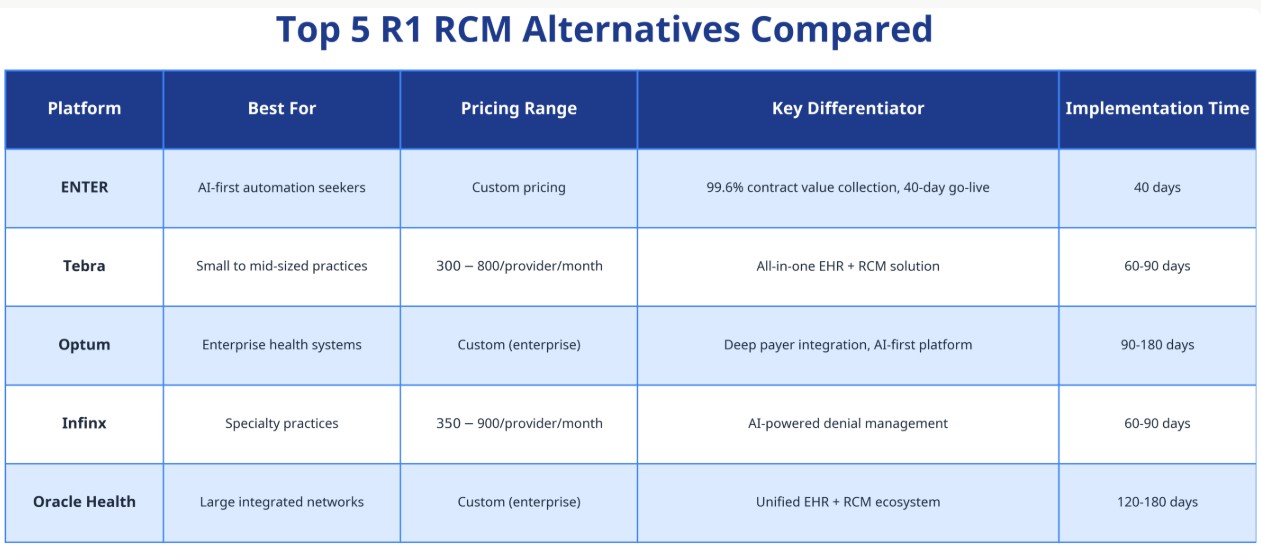
R1 RCM is a leading revenue cycle management provider with $2.46 billion in annual revenue, but its high costs ($420-$1,300/provider/month) and complex contracts drive many practices to seek alternatives. This guide compares five top R1 RCM alternatives, ENTER, Tebra, Optum, Infinx, and Oracle Health, across pricing, features, integration capabilities, and ideal use cases to help you find the best fit for your practice.
What is R1 RCM?
R1 RCM is an enterprise-grade revenue cycle management platform serving hospitals and large health systems across the United States. The company manages billing, claims processing, payment posting, and denial management for healthcare providers.
Key R1 RCM Statistics:
- Market Position: Commands 35-45% market share in the enterprise RCM segment
- Revenue: $2.46 billion TTM as of October 2025
- Pricing: $420-$1,300 per provider per month
- Target Market: Large hospitals and health systems
Why Healthcare Providers Seek R1 RCM Alternatives
Despite R1's market dominance, many practices explore alternatives for these reasons:
1. High Cost Structure
- Monthly fees of $420-$1,300 per provider create significant overhead for small to mid-sized practices
- Additional implementation and integration fees can exceed $50,000 for complex deployments
- Long-term contracts lock practices into multi-year commitments
2. Complex Implementation
- Average implementation timeline of 6-12 months
- Requires dedicated IT resources and extensive staff training
- Legacy system integration challenges reported by multiple users
3. Limited Flexibility
- Designed primarily for large enterprise environments
- Customization options limited without additional consulting fees
- Difficult to scale down for smaller practice needs
4. Customer Service Concerns
- Better Business Bureau complaints cite billing resolution delays
- Long hold times and escalation challenges reported
- Limited dedicated account management for smaller clients
Top 5 R1 RCM Alternatives Compared
1. ENTER: AI-First RCM Platform
Overview
ENTER is an AI-powered revenue cycle management platform that automates the entire billing process from claim creation to payment posting. The platform integrates with any EHR system and delivers industry-leading collection rates.
Key Features
- claimAI: Builds perfect claims without human intervention using real-time eligibility verification
- paymentAI: Posts payments in seconds from both ERAs and EOBs
- denialAI: 0% leakage with programmatic payer follow-up and AI-assisted investigation
- contractAI: Manages all contract types (fee-for-service, value-based care, workers comp)
- Custom EHR Integration: Supports any EHR with continuous integration management
Pricing
- Custom pricing based on practice size and volume
- No per-provider fees—pricing scales with collections
- 40-day implementation from contract to full automation
Best For
- Practices seeking maximum automation and minimal manual intervention
- Organizations frustrated with slow payment posting and high denial rates
- Health systems wanting to replace multiple RCM vendors with one platform
Pros & Cons
Pros:
- Industry-leading 99.6% contract value collection rate (vs. 68% industry average)
- Fastest payment posting (seconds vs. 5 days industry average)
- Zero leakage on denials and underpayments
- Transparent, real-time reporting dashboard
Cons:
- Newer market entrant (less brand recognition than R1)
- Custom pricing requires sales consultation
- Best suited for practices ready to fully automate (not hybrid models)
2. Tebra (Kareo + PatientPop): All-in-One Practice Solution
Overview
Tebra combines practice management, EHR, and RCM into a unified platform designed for independent practices and small groups. Formed from the merger of Kareo and PatientPop, Tebra emphasizes ease of use and integrated workflows.
Key Features
- Integrated EHR and practice management system
- Patient engagement tools (online scheduling, text reminders)
- Claims scrubbing and submission
- Payment processing and patient billing
- Marketing and reputation management tools
Pricing
- $300-$800 per provider per month
- Tiered pricing based on features and practice size
- Additional fees for credit card processing and patient payments
Best For
- Small to mid-sized independent practices (1-10 providers)
- Practices wanting an all-in-one EHR + RCM solution
- Organizations prioritizing ease of use over advanced automation
Pros & Cons
Pros:
- User-friendly interface with minimal training required
- Bundled EHR eliminates integration complexity
- Strong patient engagement features
- Transparent pricing tiers
Cons:
- Limited customization for complex billing scenarios
- Less robust for specialty-specific workflows
- Higher per-provider cost than standalone RCM solutions
- Fewer AI-powered automation features
3. Optum: Enterprise AI-First RCM
Overview
Optum, a UnitedHealth Group company, offers an enterprise-grade RCM platform with deep payer integration and AI-powered automation. Launched in May 2025, Optum's AI-first platform targets large health systems.
Key Features
- AI-driven claims optimization and denial prediction
- Direct payer connectivity (especially UnitedHealthcare)
- Revenue integrity and compliance monitoring
- Advanced analytics and benchmarking
- Population health integration
Pricing
- Custom enterprise pricing (typically $500,000+ annual contracts)
- Volume-based discounts for large health systems
- Implementation costs range from $100,000-$500,000
Best For
- Large health systems (100+ providers)
- Organizations with significant UnitedHealthcare volume
- Enterprises requiring deep analytics and population health integration
Pros & Cons
Pros:
- Strongest payer relationships in the industry
- Comprehensive analytics and reporting
- Proven track record with large health systems
- Integrated population health capabilities
Cons:
- Prohibitively expensive for small to mid-sized practices
- Long implementation timelines (6-12 months)
- Requires dedicated IT and RCM staff
- Less flexible for independent practices
4. Infinx: AI-Powered Denial Management Specialist
Overview
Infinx focuses on AI-powered automation for denial management, prior authorization, and patient access. The platform excels at reducing claim denials and accelerating reimbursement for specialty practices.
Key Features
- AI-driven denial prevention and appeals automation
- Prior authorization workflow automation
- Patient eligibility verification
- Revenue recovery services
- Specialty-specific coding support
Pricing
- $350-$900 per provider per month
- Performance-based pricing options available
- Additional fees for revenue recovery services
Best For
- Specialty practices with high denial rates (cardiology, orthopedics, oncology)
- Organizations struggling with prior authorization bottlenecks
- Practices seeking to reduce A/R days and improve cash flow
Pros & Cons
Pros:
- Industry-leading denial management capabilities
- Strong specialty-specific expertise
- Flexible pricing models (flat fee or performance-based)
- Faster implementation than enterprise platforms
Cons:
- Less comprehensive than full-service RCM platforms
- May require additional tools for complete revenue cycle coverage
- Newer company with less market presence than R1
- Limited EHR integration compared to larger competitors
5. Oracle Health (Cerner): Unified EHR + RCM Ecosystem
Overview
Oracle Health (formerly Cerner) offers an integrated EHR and RCM platform with 21.8% hospital market share. The platform provides seamless data flow between clinical and financial systems.
Key Features
- Native EHR integration (no third-party interfaces)
- Enterprise revenue cycle management
- Patient accounting and billing
- Contract management and compliance
- Cloud-based infrastructure with AI roadmap
Pricing
- Custom enterprise pricing (typically $1M+ for large implementations)
- Bundled EHR + RCM pricing available
- Ongoing maintenance fees of 15-20% annually
Best For
- Large hospitals and health systems already using Cerner EHR
- Organizations prioritizing clinical-financial data integration
- Enterprises with dedicated IT and RCM departments
Pros & Cons
Pros:
- Seamless EHR-RCM integration eliminates data silos
- Proven scalability for large health systems
- Strong compliance and security features
- Comprehensive training and support resources
Cons:
- Extremely high cost for small to mid-sized practices
- Long implementation timelines (12-24 months)
- Requires significant IT infrastructure and expertise
- Less flexible for practices using non-Cerner EHRs
How to Choose the Right R1 RCM Alternative
Step 1: Assess Your Practice Size and Complexity
- Small practices (1-10 providers): Consider Tebra or ENTER for ease of use and faster implementation
- Mid-sized practices (10-50 providers): Evaluate ENTER or Infinx for automation and specialty support
- Large health systems (50+ providers): Compare Optum and Oracle Health for enterprise capabilities
Step 2: Define Your Primary Pain Points
- High denial rates: Prioritize Infinx or ENTER for AI-powered denial management
- Slow payment posting: Choose ENTER for automated payment reconciliation
- Complex contracts: Look for platforms with robust contract management (ENTER, Oracle Health)
- EHR integration challenges: Select vendors with proven integration expertise
Step 3: Evaluate Total Cost of Ownership
Calculate 3-year TCO including:
- Monthly subscription or per-provider fees
- Implementation and training costs
- Integration and customization fees
- Ongoing support and maintenance
- Potential revenue improvement (collection rate increases)
Step 4: Request Demos and References
- Schedule live demos with your actual data
- Ask for references from similar-sized practices in your specialty
- Review customer satisfaction scores on G2, Capterra, and KLAS Research
- Evaluate vendor responsiveness during the sales process
Step 5: Pilot Before Full Commitment
- Negotiate a pilot period (30-90 days) if possible
- Test with a subset of providers or specialties
- Measure key metrics (collection rate, A/R days, denial rate)
- Gather staff feedback on usability and workflow impact
Market Trends Driving RCM Platform Selection
The global revenue cycle management market is experiencing rapid growth, projected to reach $105.35 billion by 2030, growing at a CAGR of 11.5%. Several trends are reshaping how practices choose RCM platforms:
1. AI-Powered Automation
The AI in healthcare RCM market is valued at $25.7 billion in 2025 and projected to reach $180.33 billion, driven by:
- Automated coding and claim generation
- Predictive denial management
- Intelligent payment posting and reconciliation
2. Value-Based Care Complexity
Practices managing multiple payment models need platforms that handle:
- Fee-for-service and capitated contracts simultaneously
- Quality metric tracking and reporting
- Risk-based contract performance monitoring
3. Patient Financial Responsibility
With patient responsibility reaching 30-40% of total collections, platforms must offer:
- Transparent cost estimates before service
- Flexible payment plans and financing options
- Digital payment portals and text-to-pay features
Frequently Asked Questions
What is the average cost of R1 RCM?
R1 RCM pricing ranges from $420 to $1,300 per provider per month, depending on practice size, specialty, and service level. Implementation costs can add $50,000-$200,000 for complex deployments.
How long does it take to switch from R1 RCM to an alternative?
Implementation timelines vary by platform:
- ENTER: 40 days from contract to full automation
- Tebra: 60-90 days, including EHR migration
- Infinx: 60-90 days for denial management focus
- Optum/Oracle Health: 90-180 days for enterprise deployments
Can I use an RCM platform without changing my EHR?
Yes, most modern RCM platforms integrate with existing EHR systems through APIs, HL7 interfaces, or custom integrations. ENTER, for example, supports any EHR with custom integration development at no additional charge.
What collection rate should I expect from an RCM platform?
Industry average collection rates hover around 68% of contract value. Top-performing platforms like ENTER achieve 99.6% of contract value, while enterprise solutions typically deliver 85-95% depending on specialty and payer mix.
Is it worth switching from R1 RCM if I'm already implemented?
Consider switching if you're experiencing:
- Collection rates below 90% of contract value
- Payment posting delays exceeding 3-5 days
- Denial rates above 10%
- Customer service response times exceeding 48 hours
- Annual cost increases above 5-7%
Calculate potential ROI by comparing your current collection rate and costs against alternative platforms' performance guarantees.
Conclusion
While R1 RCM remains a market leader in enterprise revenue cycle management, its high costs, complex implementation, and limited flexibility drive many practices to explore alternatives. The right choice depends on your practice size, specialty, automation priorities, and budget.
Quick Recommendations:
- For maximum automation and fastest ROI: ENTER offers AI-first automation with 40-day implementation
- For small practices wanting simplicity: Tebra provides an all-in-one EHR + RCM solution
- For enterprise health systems: Optum and Oracle Health deliver comprehensive platforms with deep payer integration
- For specialty practices with high denials: Infinx specializes in AI-powered denial management
Ready to Explore R1 RCM Alternatives?
The RCM market is evolving rapidly, with AI-powered platforms delivering collection rates and automation levels that were impossible just 2-3 years ago. Schedule demos with 2-3 platforms that match your practice profile, and use the comparison framework in this guide to evaluate which solution best addresses your specific pain points.
Next Steps:
- Calculate your current RCM total cost of ownership
- Identify your top 3 pain points (denials, payment posting, integration, etc.)
- Request demos from platforms that specialize in solving those challenges
- Negotiate pilot periods to test performance before full commitment


