Talk to Sales
HL7 Integration Costs: Why They're So Expensive + Ways to Reduce Them
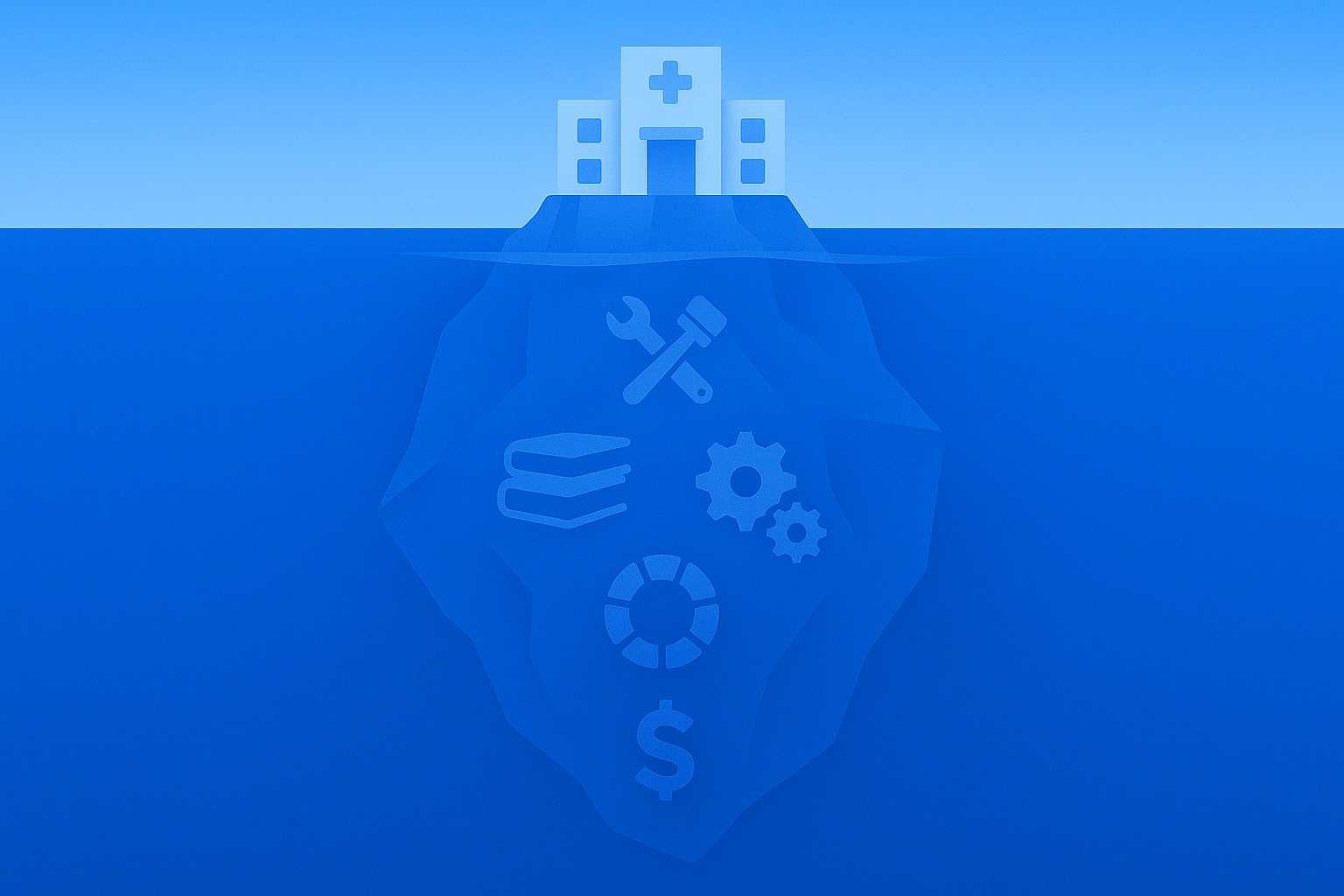
Healthcare organizations are losing significant revenue to hidden HL7 integration costs that can spiral into millions of dollars in unplanned expenses. According to recent industry analysis, healthcare facilities can spend anywhere from $48,000 to $58,000 on electronic health record (EHRs) solutions, with HL7 integration representing a substantial portion of these costs. The reality is more costly than expected, many providers enter HL7 projects anticipating straightforward implementation costs, only to discover that annual maintenance alone can consume 15-20% of the initial EHR investment.
This financial burden becomes even more severe when you consider that over 50% of the total cost of ownership for most healthcare software accumulates through ongoing support and maintenance.
The complexity of HL7 integration extends far beyond simple data exchange. It includes version compatibility issues, custom EHR configurations, and long-term support costs, all of which drive costs higher than most organizations anticipate. With over 95% of U.S. healthcare organizations already utilizing HL7 standards developed by Health Level Seven International, the pressure to implement and maintain these systems effectively has never been greater.
Key Factors Influencing HL7 Integration Costs
The financial impact of HL7 integration stems from multiple interconnected factors that healthcare organizations often underestimate during the initial planning phases. The complexity of the EHR system serves as the primary cost driver, as healthcare providers must integrate disparate systems that were never designed to communicate seamlessly. The heterogeneous nature of healthcare IT infrastructure means that each integration project requires custom development, specialized expertise, and extensive testing to ensure data integrity and regulatory compliance.
Data exchange complexity adds another layer of cost to HL7 integration projects. Healthcare providers must ensure that patient information flows accurately between electronic medical records (EMRs), billing systems, laboratory information systems (LIS), and other critical healthcare IT components. The challenge intensifies when organizations need to support multiple HL7 versions simultaneously, as legacy systems may rely on older standards while newer applications require modern Fast Healthcare Interoperability Resources (FHIR) capabilities.
Challenges and Considerations in HL7 Integration
Healthcare organizations face significant technical and operational challenges that directly impact HL7 integration costs and long-term success. The industry's reliance on legacy systems compounds these challenges, as older EHR platforms may lack the technical capabilities needed to support modern HL7 standards without substantial upgrades or even full replacements.
Variance in Implementation Standards
The lack of standardized HL7 implementation approaches across healthcare vendors creates a costly fragmentation problem that organizations must navigate carefully. EHR vendors interpret HL7 standards in inconsistent ways, leading to compatibility issues that require custom interface development and ongoing maintenance. Healthcare providers often discover that systems from different vendors cannot communicate effectively, despite both claiming HL7 compliance, forcing them to invest in specialized integration expertise and custom coding solutions.
The cost breakdown for these customizations often highlights the limitations of HL7 V2, which is sometimes called a "non-standard standard" because roughly 80% of an interface might follow the specification, while the remaining 20% requires extensive customization.
Risks in Electronic Health Record Migration
EHR migration projects represent one of the highest-risk and most expensive aspects of HL7 integration, with potential costs reaching $1.5 million per violation for compliance failures during the transition. Healthcare organizations must carefully plan migration strategies that maintain data integrity while ensuring the continuous operation of critical clinical and administrative systems.
The complexity of transferring years or decades of patient information while maintaining HL7 compliance demands specialized expertise, thorough testing, and multi-phase rollouts that often span over several months or even years.
Unreliable Data Semantics
Semantic consistency presents a major challenge when organizations attempt to maintain meaning and context across different systems and HL7 versions. Clinical data must retain its original intent while supporting complex workflows that cross departmental and organizational boundaries.
Healthcare organizations often invest in custom features and specialized coding to ensure that HL7 interfaces meet unique operational needs while remaining compliant with regulatory and interoperability standards.
Evaluating Different HL7 Versions
The choice of HL7 version significantly impacts both initial implementation costs and long-term maintenance expenses, making version selection a critical financial decision for healthcare organizations. Each HL7 version offers different capabilities and complexity levels that directly influence development costs, ongoing support requirements, and integration flexibility.
Understanding HL7 V2 and Its Cost Implications
HL7 V2 remains the most widely adopted standard in healthcare, offering a balance of functionality and implementation simplicity that makes it attractive for many organizations. The mature ecosystem surrounding HL7 V2 provides access to experienced developers, established interface engines, and proven implementation methodologies that can reduce both initial costs and implementation risks.
However, the "non-standard standard" nature of HL7 V2 means that organizations must budget for significant customization work, as approximately 20% of each interface typically requires site-specific modifications to achieve full functionality.
Examining HL7 V3: Benefits and Drawbacks
HL7 V3 addresses many of the limitations inherent in the V2 standard by providing a more structured and semantically rich framework for healthcare data exchange. The Reference Information Model (RIM) that underlies HL7 V3 provides a comprehensive conceptual framework for healthcare information, supporting more precise data representation and improved interoperability between different clinical domains.
However, the complexity of HL7 V3 has limited its adoption—particularly among smaller healthcare organizations that lack the technical infrastructure or resources needed to support its implementation.
HL7 CDA: Costs and Considerations
HL7 Clinical Document Architecture (CDA) provides a framework for standardizing clinical document formats and content, but implementation requires careful attention to local workflow requirements and documentation practices. Healthcare organizations must balance the benefits of standardization with the need to maintain clinical workflow efficiency and provider satisfaction.
The most successful CDA implementations involve clinical stakeholders early in the design process to ensure standardized formats support rather than hinder clinical care delivery.
Exploring HL7 FHIR: Modern Approach and Associated Costs
HL7 FHIR represents the newest evolution in healthcare interoperability standards, offering REST APIs and modern web technologies that can reduce development costs and improve integration flexibility. As of 2025, nearly 90% of global health systems have implemented FHIR-enabled APIs, with 84% of healthcare leaders expecting continued growth in FHIR adoption.
FHIR’s modern architecture allows healthcare organizations to leverage existing web development expertise and tools, potentially lowering the specialized knowledge requirements that often drive up HL7 integration costs.
The Benefits of HL7 Integration
Despite the significant costs associated with HL7 implementation, healthcare organizations that successfully deploy these standards achieve substantial operational and financial benefits that justify the investment. The standardization enables healthcare providers to focus on patient care rather than managing complex data integration challenges.
Improved Efficiency in Healthcare Processes
HL7 integration eliminates manual data entry processes and reduces administrative burden across healthcare organizations. When EHR systems can automatically transmit patient information, insurance coverage details, and clinical documentation to billing systems through standardized HL7 messages, the risk of transcription errors drops significantly. This automation extends to insurance verification, where real-time HL7-enabled queries can validate coverage and benefits before services are rendered, preventing downstream denials and reducing administrative rework.
Enhanced Patient Care and Outcomes
HL7 standards enable healthcare providers to access comprehensive patient information regardless of which system originally captured the data, supporting better clinical decision-making and care coordination. The integration supports clinical decision support tools, automates regulatory reporting, and enables integration with telehealth platforms and mobile health apps. Healthcare teams can collaborate more effectively when patient information flows seamlessly between different departments and external partners through RCM platforms.
Compliance with Standards and Regulations
HL7 integration provides healthcare organizations with improved regulatory compliance capabilities, reduced administrative costs, and better support for revenue cycle management processes. The standardization ensures that audit trails and documentation requirements are consistently met across workflows while supporting compliance with evolving regulatory requirements and protecting against cybersecurity threats.
Comparing Integration Methods: Point-to-Point vs. HL7 Engines
The choice between point-to-point interfaces and comprehensive HL7 integration engines represents a fundamental decision that significantly impacts both initial costs and long-term maintenance expenses.
Cost Analysis of Traditional Point-to-Point Interfaces
Traditional point-to-point interfaces appeal to healthcare organizations seeking to minimize initial integration costs, as they require less sophisticated infrastructure and can be implemented more quickly than comprehensive integration platforms. However, the cost advantage of point-to-point approaches often proves illusory, as healthcare organizations discover the exponential growth in complexity and maintenance costs as they add new systems and interfaces. Each point-to-point connection requires individual development, testing, and maintenance, creating a web of dependencies that becomes increasingly expensive and difficult to manage over time.
Advantages of Modern HL7 Integration Engines
Modern HL7 integration engines provide centralized management capabilities that can significantly reduce long-term integration costs while improving reliability and scalability. These platforms offer sophisticated routing, transformation, and monitoring capabilities that enable healthcare organizations to manage complex integration scenarios through a single interface. The centralized approach reduces the specialized expertise required for interface management and enables healthcare organizations to leverage economies of scale when adding new systems or modifying existing integrations.
Ongoing Maintenance and Technical Support Costs
The long-term financial commitment of HL7 integration extends far beyond initial implementation costs to encompass ongoing maintenance, security patching, and technical support requirements.
Importance of Regular Updates and System Support
Healthcare organizations should set aside approximately 20% of their integration budget each year to cover routine maintenance, security patching, monitoring, regulatory-driven upgrades, and infrastructure refreshes as hardware ages. The complexity of HL7 systems means that maintenance activities often require specialized expertise that may not be available internally, pushing healthcare organizations to rely on expensive vendor support or specialized consulting services.
Strategies for Cost-Effective Maintenance
Training and user adoption represent another significant component of ongoing HL7 costs that healthcare organizations often underestimate. As healthcare teams adapt to new workflows and system capabilities, organizations must invest in comprehensive training programs and ongoing support which is why contract compliance management software integration becomes crucial for cost control.. The complexity of modern healthcare IT environments means that staff turnover can create recurring training costs, particularly for specialized roles that require deep understanding of HL7 standards and custom system configurations.
Total Cost of Ownership in HL7 Integration
Understanding the complete financial picture of HL7 integration requires careful analysis of all cost components throughout the system lifecycle. The total cost of HL7 integration extends beyond implementation to include ongoing support, training, and maintenance—areas where ENTER’s modern RCM platform helps reduce complexity and streamline operations. Additionally, understanding how contract compliance management software integrates with HL7 systems can help organizations achieve better cost control and operational efficiency.
Frequently Asked Questions
What is HL7 in healthcare?
HL7 (Health Level Seven) is a set of international standards for the exchange, integration, sharing, and retrieval of electronic health information. Developed by Health Level Seven International, HL7 enables different healthcare systems to communicate effectively—supporting everything from electronic health records to billing systems and clinical decision support tools.
What are the benefits of HL7?
HL7 integration provides numerous benefits, including improved patient care through better data sharing, enhanced operational efficiency via automated data exchange, and reduced medical errors through standardized information formats. It also supports regulatory compliance, lowers administrative costs, and strengthens revenue cycle management capabilities.
What does HL7 integration mean?
HL7 integration refers to the process of connecting different healthcare systems using HL7 standards to enable seamless data exchange. This allows EHRs, LIS, billing systems, and other healthcare applications to share patient information automatically, eliminating the need for manual data entry and reducing the risk of errors.
What does HL7 enable clinical systems to do?
HL7 enables clinical systems to share patient information in real-time, support clinical decision support tools, automate regulatory reporting, and integrate with telehealth platforms and mobile health apps. It allows providers to access complete patient information regardless of the system in which is originated, improving decision-making and care coordination.
Why is HL7 integration so expensive?
HL7 integration can be costly due to factors like custom interface development, legacy system compatibility, version fragmentation, and ongoing maintenance requirements. Costs are further influenced by the complexity of EHR systems, the number of systems being integrated, and the need for specialized technical expertise to ensure secure, compliant data exchange.


