Talk to Sales
Denial Management Software vs Waystar: Which Solution Fits Your Practice?

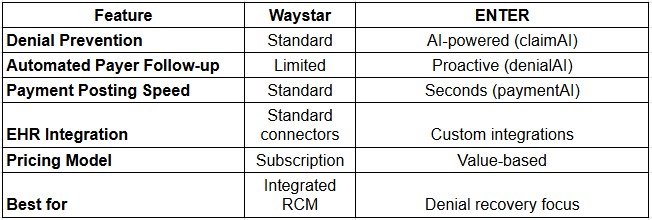
Waystar excels in claims management and payer connectivity, while ENTER specializes in AI-powered denial recovery with automated follow-up. Choose Waystar for broad RCM functionality; choose ENTER if denial prevention and underpayment recovery are your top priorities.
What Is Denial Management Software?
Denial management software automates the process of tracking, analyzing, and recovering denied claims. Instead of manual follow-up, these tools identify why claims were denied and take action either resubmitting or appealing to payers.
Key functions:
- Tracks denied and rejected claims in real-time
- Categorizes denial reasons (coding, missing documentation, eligibility)
- Automates resubmission and appeals
- Monitors payer response times
- Recovers underpayments and partial denials
The average medical practice loses 15–25% of claims revenue to denials, making denial management critical for cash flow. In fact, claim denials cost U.S. healthcare providers over $262 billion annually, with denial rates increasing by 3-5% year-over-year across most specialties.
Waystar: Overview & Strengths
Waystar is a cloud-based RCM platform focused on claims management and payer connectivity. It serves mid-sized to large healthcare organizations.
What Waystar does well:
- Broad RCM integration: Handles claims, eligibility, and payment posting in one platform
- Payer connectivity: Direct connections to 500+ payers for faster claims submission
- Claims visibility: Real-time tracking of claims status across payers
- Customizable workflows: Flexible rules engine for different practice types
- Established market presence: Used by thousands of healthcare organizations
Best for: Multi-location practices needing integrated RCM and broad payer connectivity.
ENTER: Overview & Strengths
ENTER is an AI-first RCM platform emphasizing denial prevention and automated recovery through its denialAI engine.
What ENTER does well:
- AI-powered denial prevention: claimAI builds claims with 99.6% accuracy, reducing denials at the source
- Automated denial follow-up: denialAI proactively contacts payers on your behalf—0% leakage guarantee
- Payment automation: paymentAI posts payments in seconds, not days
- Custom EHR integration: Seamless connection to any EHR system
- Transparent pricing: Value-based model tied to recovery performance
Best for: Practices prioritizing denial prevention and maximizing revenue recovery.
Head-to-Head Comparison
Key Differences Explained
1. Denial Prevention Approach
Waystar: Uses standard rules-based claim validation. Claims are checked against basic coding and documentation standards before submission.
ENTER: Uses AI (claimAI) to build near-perfect claims. The system learns from your practice's data and payer requirements, reducing denials before they happen.
Why it matters: Preventing denials is cheaper than recovering them. ENTER's focus here saves time and money.
2. Payer Follow-up
Waystar: Provides visibility into claim status. You manage follow-up with payers manually or through your staff.
ENTER: denialAI automatically contacts payers, negotiates underpayments, and escalates denials. No staff involvement needed.
Why it matters: Automated follow-up means faster recovery and zero missed opportunities.
3. Payment Posting
Waystar: Standard payment posting workflow. Payments are manually reconciled against claims.
ENTER: paymentAI posts all payments (ERAs, EOBs) in seconds and auto-reconciles against contracts. Identifies underpayments instantly.
Why it matters: Faster posting = faster cash flow and immediate visibility into payment issues.
4. ntegration Approach
Waystar: Pre-built connectors to major EHRs (Epic, Cerner, Athena). Works well if you use a supported system.
ENTER: Custom EHR integrations. Pulls billing data directly from your EHR, regardless of system.
Why it matters: Custom integration means deeper data access and fewer manual workarounds.
Pricing & ROI
Waystar: Subscription-based pricing, typically $2,000–$5,000+ per month depending on volume and modules.
ENTER: Value-based pricing. You pay based on revenue recovered. Average practices see 20–30% improvement in net collections.
ROI comparison:
- Waystar: Fixed cost, predictable budget
- ENTER: Variable cost, tied to performance
According to industry benchmarks, practices implementing automated denial management see ROI within 6-9 months, with some seeing payback periods as short as 90 days when combined with AI-powered claim validation.
When to Choose Each
Choose Waystar if:
- You need broad RCM functionality (claims, eligibility, payments, reporting)
- Your practice uses Epic, Cerner, or Athena
- You prefer a subscription pricing model
- You have an in-house billing team to manage denial follow-up
Choose ENTER if:
- Denial prevention and recovery are your top priorities
- You want to reduce billing staff workload
- You use a non-standard EHR system
- You prefer paying for results, not features
Research shows that practices using AI-powered denial management recover claims 40% faster than those using manual processes, directly impacting your bottom line.
Implementation Timeline
Waystar: 6–8 weeks (standard EHR integration) to 12+ weeks (custom workflows)
ENTER: 4 weeks (40-day onboarding) from contract to full automation
Conclusion
Both Waystar and ENTER are strong denial management solutions. Waystar wins on breadth and integration flexibility; ENTER wins on denial prevention and automation. Your choice depends on whether you prioritize integrated RCM or focused denial recovery.
Ready to reduce denials and recover more revenue? Request a demo with ENTER to see how denialAI can work for your practice.
Frequently Asked Questions
Can I use both Waystar and ENTER together?
Yes. Some practices use Waystar for broad RCM and layer ENTER on top for denial-specific automation.
Does ENTER work with my EHR?
ENTER develops custom integrations for any EHR. Contact their team to confirm compatibility.
How long will it take to see ROI with ENTER?
Most practices see measurable improvement in 30–60 days. Full automation takes 40 days.
What if I'm already using Waystar?
You can migrate to ENTER or use both. ENTER's team handles the transition.


