Talk to Sales
Thank you! Your submission has been received!
Oops! Something went wrong
Just
CTRL
ENTER
It
Just CTRL ENTER It With These Prompts
Executives
Prompt
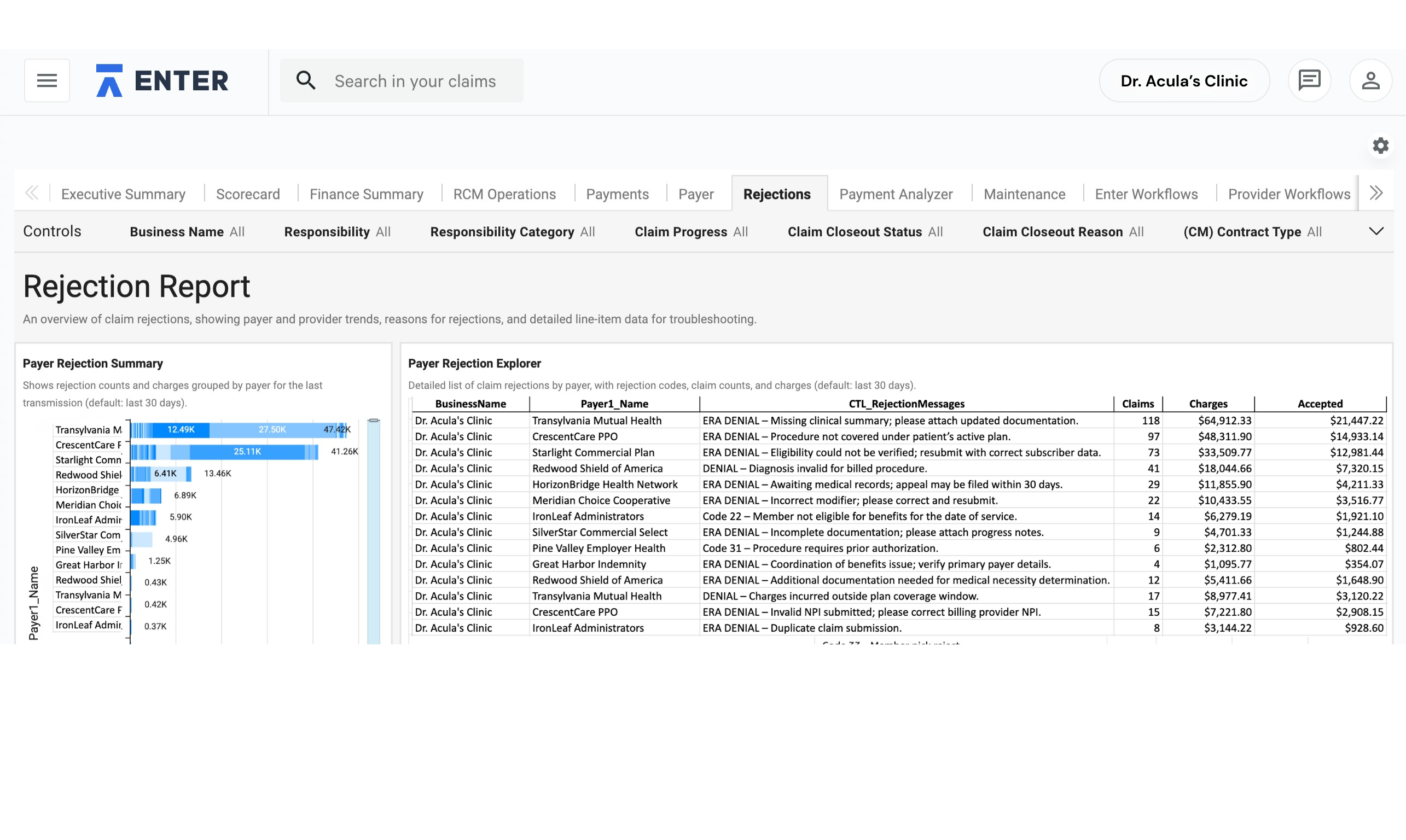
What’s driving the drop in revenue this quarter?
Context
No items found.
Context
Answer
Billing Managers
Prompt
Please update the primary payer on claim ABC123 to Cigna.
Context
No items found.
Context
Answer
Billing Managers
Front Desk
Prompt
Create a message to the support team about Claim [ID Number].
Context
No items found.
Context
Answer
Billing Managers
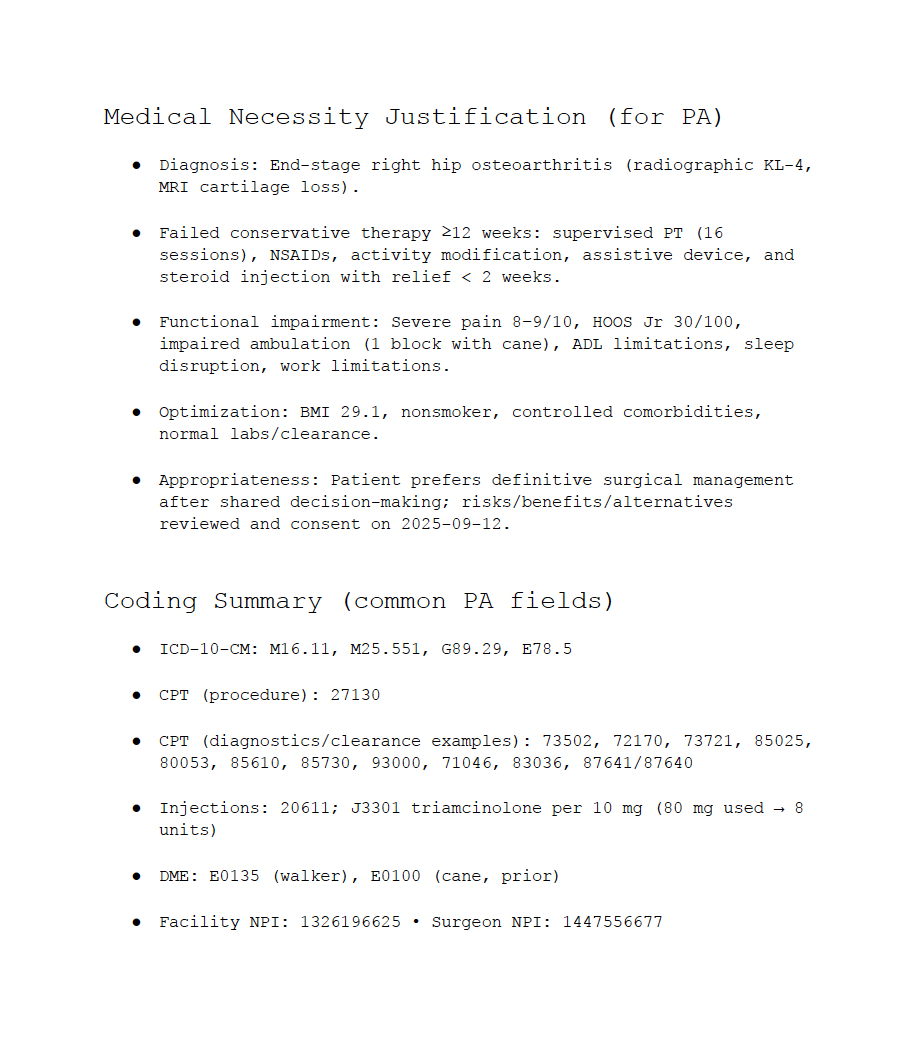
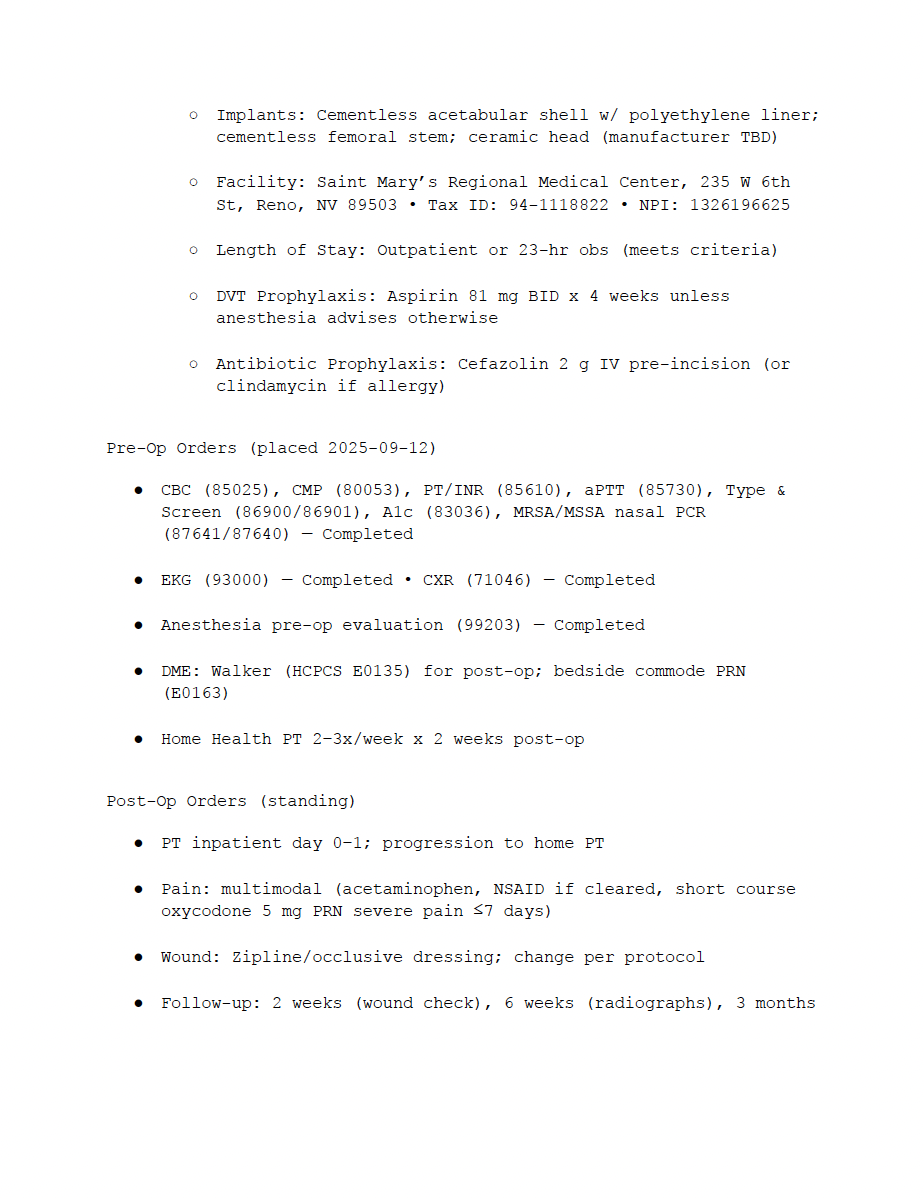
Prompt
What contract/chargemaster governs today’s DOS?
Context
No items found.
Context
Answer
Billing Managers
Prompt
What payments has John Doe made this year?
Context
No items found.
Context
Answer
Billing Managers
Prompt
What payments has John Doe made this year?
Context
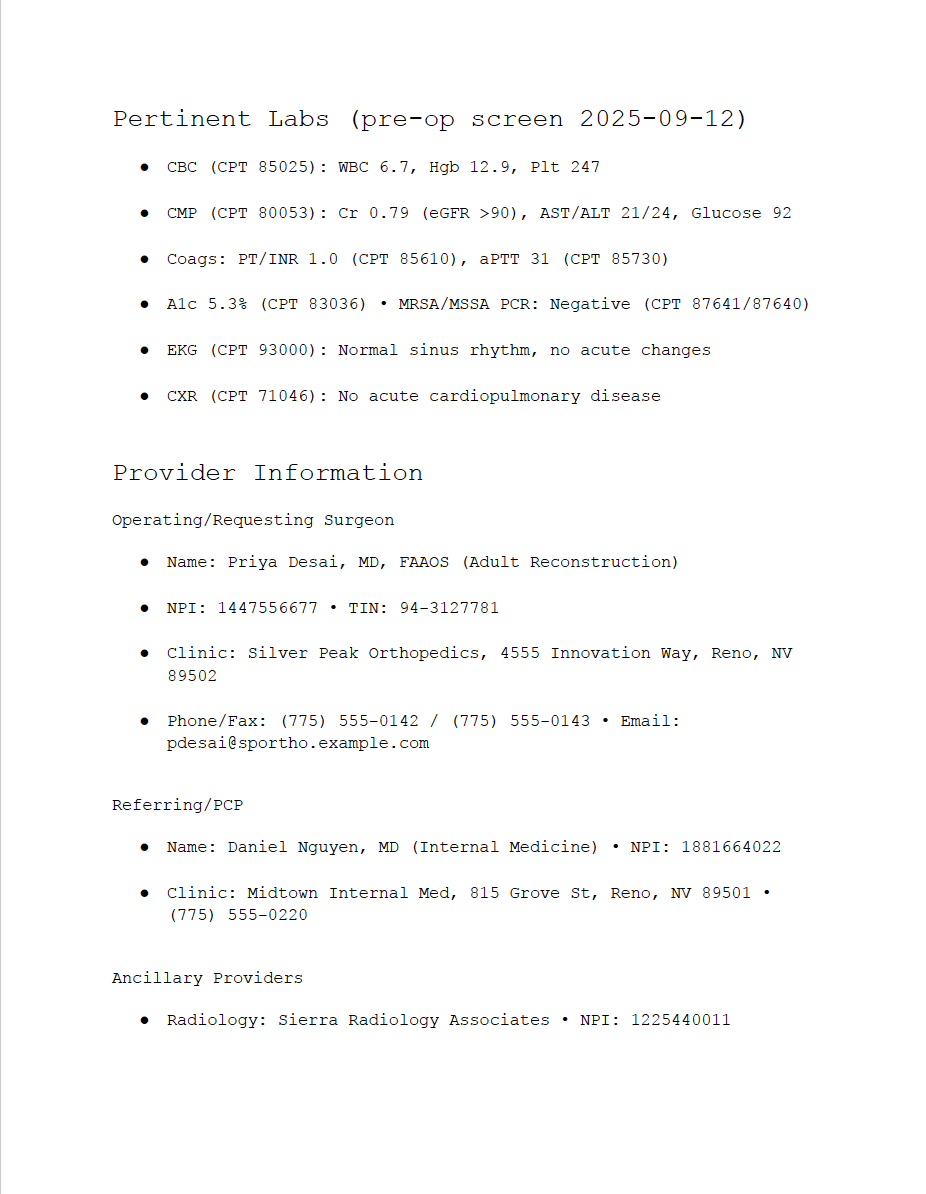
Screenshot of Patient Collection information.
No items found.
Context
Answer
Billing Managers
Prompt
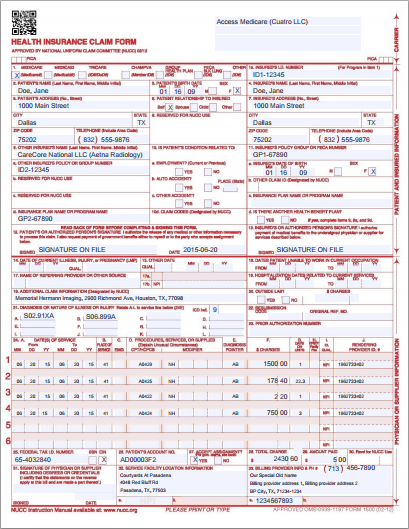
What’s the status of Claim [ID Number]?
Context
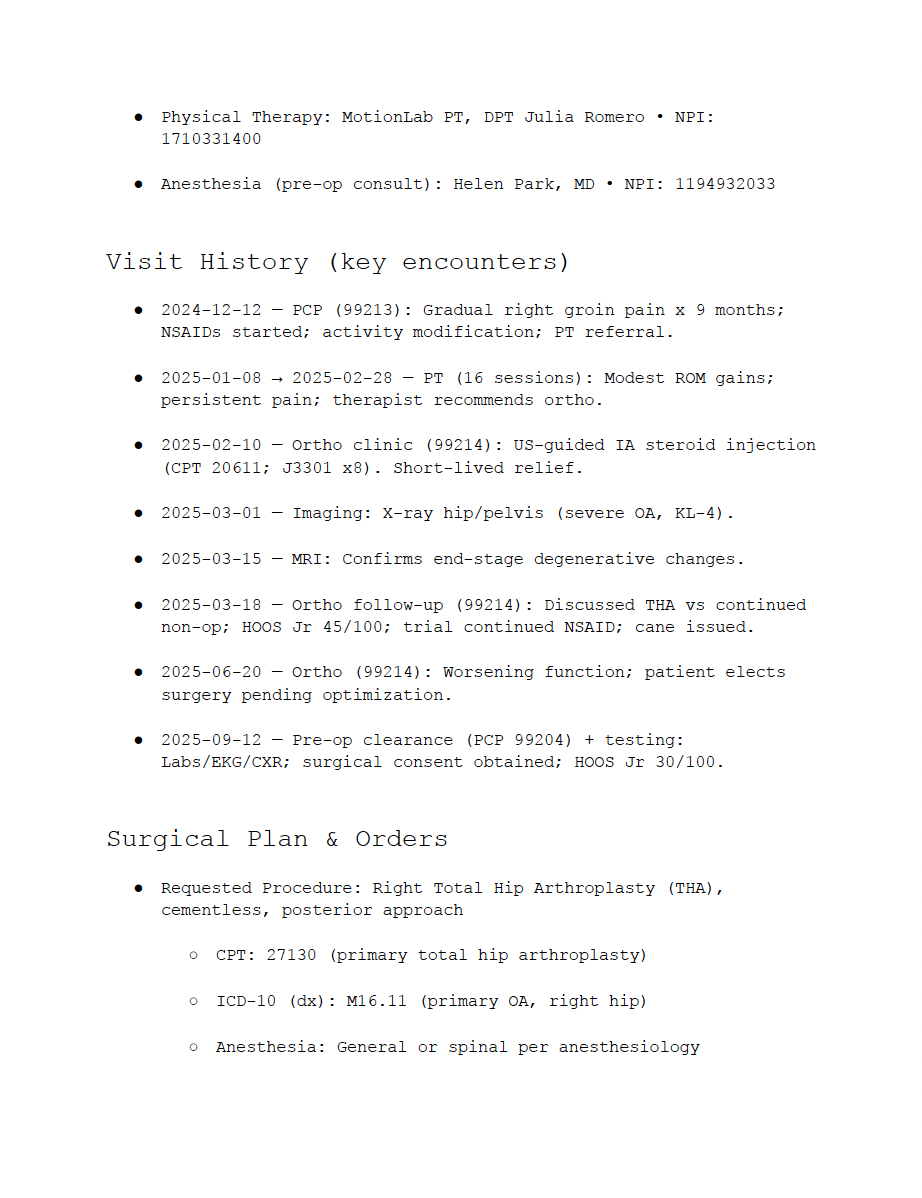
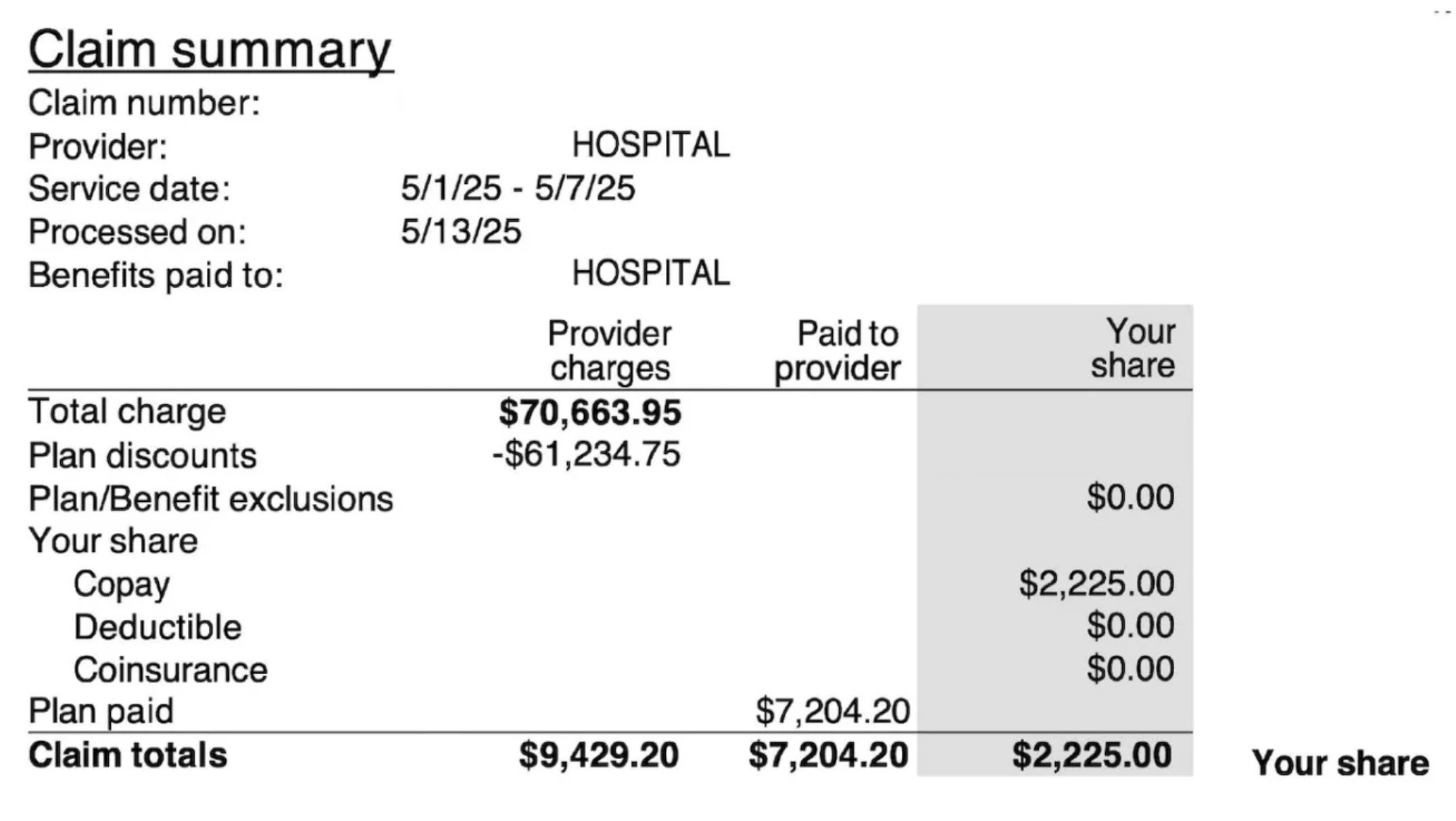
Screenshot or document of claim information
No items found.
Context
Answer
Front Desk
Billing Managers
Prompt
How much does [patient name] owe right now?
Context
No items found.
Context
Answer
Front Desk
Billing Managers
Prompt
Show me all claims for John Doe between 2024-07-01 and 2024-07-31
Context
No items found.
Context
Answer
Connect to the ENTER RCM Platform For Instant Data Access
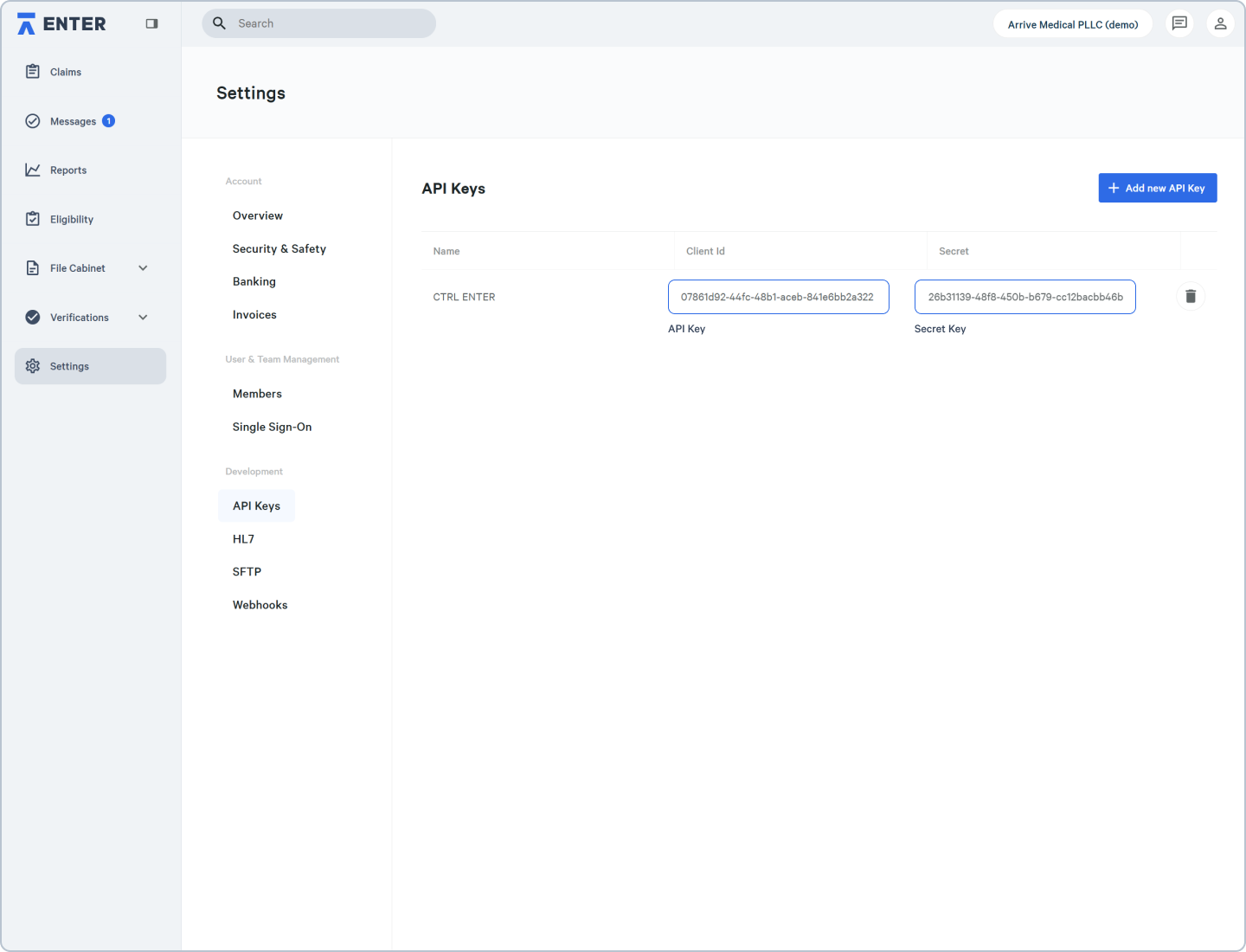
Part 1: ENTER Platform
- Download CTRL ENTER
- Open your ENTER RCM platform and navigate to Settings → Development → API Keys
- Locate your CTRL ENTER API and Secret Keys
- Copy your API key and Secret Key
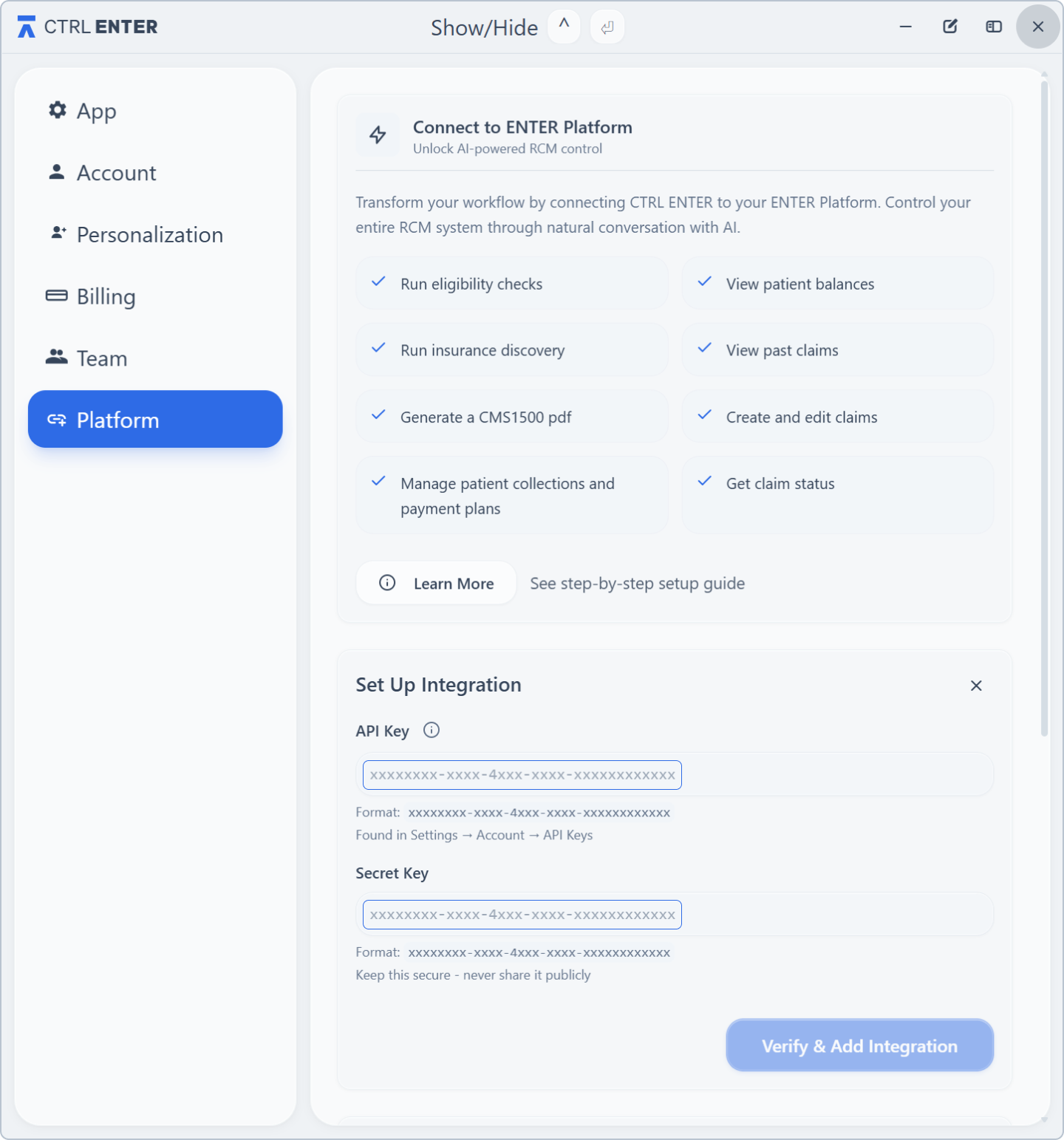
Part 2: CTRL ENTER
- Open CTRL ENTER and click the 3 dots on the top right corner of the CTRL ENTER window
- Navigate to Platform
- Under Set Up Integration, paste your keys into their respective key fields
- Click Save